The diagnosis and documentation of respiratory failure continues to be challenging for coders, documentation specialists, and physicians. Many physicians, including some intensivists and pulmonologists, are unaware of the widely recognized clinical standards for diagnosing acute respiratory failure even though multiple clinical criteria and appropriate management of respiratory failure are often clearly documented in the medical record. In this article, we will discuss a variety of clinical indicators and tools to identify respiratory failure.
Acute respiratory failure is classified as hypoxemic (low arterial oxygen levels), hypercapnic (elevated levels of carbon dioxide gas), or a combination of the two. In most cases one or the other predominates.
Most patients with acute respiratory failure demonstrate either impaired ventilation or impaired oxygen exchange in the lung alveoli.
- Impaired ventilation, as in COPD or asthma, requires increased effort to ventilate the lungs. It is characterized by hypercapnia (increased pCO2) with variable degrees of hypoxemia (low oxygen levels) and pH < 7.35 (respiratory acidosis).
- Impaired oxygen exchange in the alveoli, as in pneumonia, pulmonary edema, or pulmonary embolism, primarily causes hypoxemia (low oxygen levels), with decreased pCO2 and increased pH > 7.45 (respiratory alkalosis).
In some cases, like head trauma, drug overdose, or over-sedation, the brain’s respiratory center is suppressed causing reduced respiratory drive with decreased ventilation that may progress to respiratory arrest.
For a patient to have acute respiratory failure, it must be symptomatic and meet diagnostic criteria based on arterial blood gas (ABG) or pulse oximetry readings (SpO2).
Get our CDI Pocket Guide® for more information about acute and chronic respiratory failure.
Blood Gas Measurements
Arterial blood gas (ABG) and pulse oximetry (SpO2) are two methods of measuring blood gases. Let’s first define what they are:
| Measure |
Definition |
Normal |
| pO2 |
Partial pressure of oxygen, or oxygen content, in mmHg |
pO2 > 80 mmHg |
| pCO2 |
Partial pressure of carbon dioxide, or carbon dioxide content, in mmHg |
35 – 45 mmHg |
| pH |
Measure of the degree of acidity |
7.35 – 7.45 |
| SaO2 |
Oxygen saturation (percent of hemoglobin carrying oxygen) as reported on ABG and is relatively proportional with pO2 |
> 95% |
| SpO2 |
Oxygen saturation (percent of hemoglobin carrying oxygen) as measured by pulse oximetry and is relatively proportional with pO2 |
> 95% |
| FIO2 |
Percent of supplemental oxygen expressed as a decimal, e.g., 40% oxygen = 0.40. |
Room air = 20% = 0.20 |
| P/F ratio |
pO2 / FIO2 |
> 400 |
Next, what are the degrees of hypoxemia based on pO2 and/or SpO2 measured on room air, or the P/F ratio measured on supplemental oxygen.
| Measure |
Normal |
Hypoxemia |
Acute respiratory failure |
| pO2 (room air) |
> 80 mmHg |
60-80 mmHg |
< 60 mmHg |
| SpO2 (room air) |
> 95% |
91-95% |
< 91% |
| P/F Ratio (on oxygen) |
> 400 |
300-400 |
< 300 |
Hypoxemic Respiratory Failure
Diagnostic criteria:
- pO2 < 60 mmHg (SpO2 < 91%) on room air, or
- P/F ratio < 300, or
- 10-15 mmHg decrease from baseline (if known)
Important: P/F ratio and room air pO2/SpO2 criteria are not valid with oxygen-dependent chronic hypoxemic respiratory failure, but pO2/SpO2 criteria are valid for such patients when measured while breathing their usual home O2 flow rate or higher.
The gold standard for the diagnosis of acute hypoxemic respiratory failure is an arterial pO2 on room air less than 60 mmHg measured by arterial blood gases (ABG). In the absence of an ABG, SpO2 less than 91% measured by pulse oximetry on room air can serve as a substitute for the pO2 because SpO2 of 91% equals pO2 of 60 mmHg.
These criteria may not apply to patients with chronic hypoxemic respiratory failure (e.g., due to severe COPD), because their room air pO2 would always be expected to be < 60 mmHg (SpO2 < 91%). Chronic respiratory failure patients only qualify for home oxygen when their SpO2 is less than 91% and they are treated with supplemental oxygen on a continuous outpatient basis that is adjusted to keep arterial oxygen saturation above 92%.
Hypercapnic Respiratory Failure
Diagnostic criteria:
- pCO2 > 50 mmHg with pH < 7.35*, or
- If baseline pCO2 is known, a 10-15 mmHg increase in baseline pCO2
*A normal pH of 7.35-7.45 indicates chronic hypercapnic respiratory failure only.
The hallmark of acute hypercapnic respiratory failure is elevated pCO2 due to acute retention/accumulation of carbon dioxide gas resulting in an acidic pH less than 7.35. There are many causes, but severe COPD is the most common.
Physicians may identify these findings as “respiratory acidosis,” which is the same thing as hypercapnic respiratory failure. Respiratory acidosis and acute respiratory acidosis are indexed as hypercapnic respiratory failure and acute hypercapnic respiratory failure, respectively.
Finally, an exacerbation of symptoms requiring an increase in chronic supplemental oxygen indicates an “acute exacerbation” of chronic respiratory failure, which would be classified as acute-on-chronic respiratory failure if properly documented.
With the exception of P/F ratio, Coding Clinic, Third Quarter 1988, p. 7 and Second Quarter 1990, p. 20 have identified the above diagnostic criteria for acute hypoxemic and hypercapnic respiratory failure to assist coders and documentation specialists with the recognition of these conditions.
Symptoms
In addition to the diagnostic criteria above, any patient with acute respiratory failure would be expected to exhibit some degree of respiratory difficulty. This may be nothing more than dyspnea, tachypnea (respirations > 20), decreased respirations (<10) or wheezing, but may progress to labored breathing, nasal flaring, grunting, accessory muscle use, retractions, cyanosis and eventually respiratory arrest.
Management of Respiratory Failure
Patients with respiratory failure are treated and managed with supplemental oxygen. Supplemental oxygen may be administered by mask or nasal cannula. A Venturi mask (Venti-mask) delivers a controlled flow of oxygen at a specific fixed concentration (FIO2): 24%, 28%, 31%, 35%, 40%, and 50%. The nonrebreather (NRB) mask is designed to deliver approximately 100% oxygen. Other modalities may include steroids, inhaled bronchodilators, mucolytics and respiratory therapy.
Management that requires endotracheal intubation and mechanical ventilation or initiation of biphasic positive airway pressure (BiPAP) nearly always means the patient has acute respiratory failure, but these measures are not required for the diagnosis. Similarly, providing 40% or more supplemental oxygen implies that the physician is treating acute respiratory failure since only a patient with acute respiratory failure would need that much oxygen.
Using the P/F Ratio to Identify Acute Respiratory Failure
A frequent problem faced by coding and documentation specialists is identifying acute respiratory failure when there are no pulse oximetry measurements on room air, the patient’s symptoms are relieved after oxygen is started, or there was no ABG performed.
The P/F ratio is a powerful objective tool to identify and confirm acute hypoxemic respiratory failure at any time while the patient is receiving supplemental oxygen. The P/F ratio is easy to calculate when ABG is available since it includes the pO2 and FIO2.
The P/F ratio is calculated by dividing the pO2 by the FIO2 from the ABG. For example, pO2 is 70 and FIO2 is 0.40. P/F Ratio: 70 / 0.40 = 175. A P/F ratio < 300 indicates acute respiratory failure.
The P/F ratio indicates what the expected room air pO2 would be if oxygen were discontinued:
| P/F ratio on oxygen of |
= pO2 on room air of |
| 300 |
60 mmHg |
| 250 |
50 mmHg |
| 200 |
40 mmHg |
| 150 |
30 mmHg |
When the ABG is not available. When the pO2 is unknown because an ABG was not performed, the pulse oximetry readings (SpO2) can be used to calculate the P/F ratio.
The SpO2 can be used as a surrogate to approximate the pO2 as shown below:
SpO2
(percent) |
pO2
(mmHg) |
| 86 |
51 |
| 87 |
52 |
| 88 |
54 |
| 89 |
56 |
| 90 |
58 |
| 91 |
60 |
| 92 |
64 |
| 93 |
68 |
| 94 |
73 |
| 95 |
80 |
| 96 |
90 |
Note: The SpO2/pO2 conversion becomes unreliable when SpO2 is > 97%.
Determining FIO2 from Nasal Cannula Flow Rate. A nasal cannula provides oxygen at adjustable flow rates in liters of oxygen per minute (L/min or LPM). The actual FIO2 (percent oxygen) delivered by nasal cannula is somewhat variable and less reliable than with a mask, but can be estimated as shown below. Room air is assumed to be FIO2 of 20%.
| Flow Rate (liters/minute) |
FIO2 |
| 1 |
24% |
| 2 |
28% |
| 3 |
32% |
| 4 |
36% |
| 5 |
40% |
| 6 |
44% |
Example
A patient has SpO2 of 95% on 5 liters of oxygen. Based on the above information, the SpO2 of 95% is equal to a pO2 of 80 mmHg. Five L/min of oxygen = 40% (FIO2 = 0.40).
P/F ratio = 80 / 0.40 = 200
Although the patient may be stable and asymptomatic receiving 40% oxygen, the patient still has acute respiratory failure. If supplemental oxygen were withdrawn, the room air pO2 would only be about 40 mmHg (see above), significantly less than the diagnostic criteria of < 60 mmHg on room air.
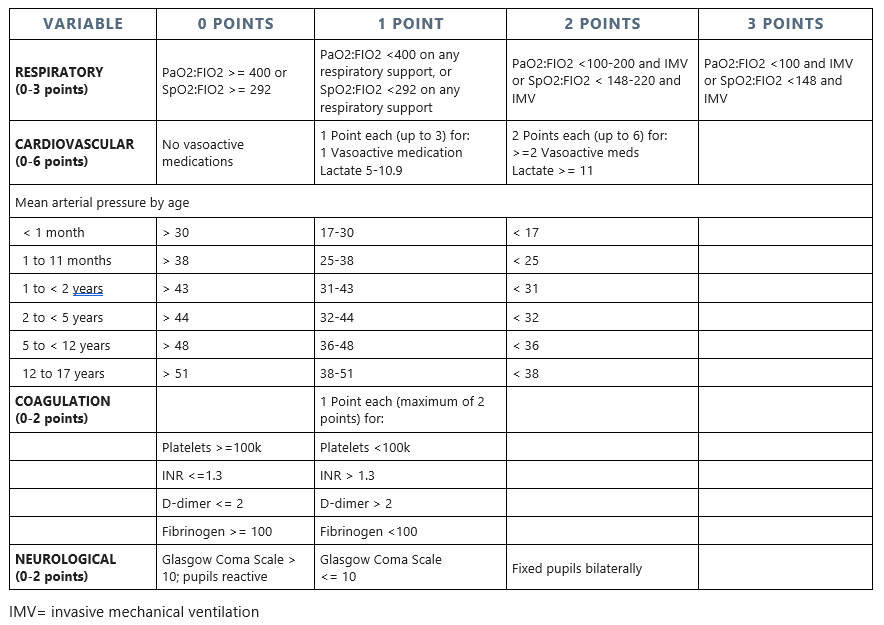
It is important to note that the P/F ratio is one of the SOFA score diagnostic criteria for Sepsis-3. Calculation of the P/F ratio on room air may be used for Sepsis-3 Respiratory SOFA scoring at the 1-point level (P/F = 300-399). Since these patients do not have respiratory failure, oxygen may not be administered. To calculate the P/F on room air an FIO2 of 20% (0.20) is used as the denominator. A P/F ratio of 300-399 indicates hypoxemia and equals 1 point on the SOFA scale; < 300 represents hypoxemic respiratory failure equaling 2 points if baseline is above 400.
Post-procedural Acute Respiratory Failure
The diagnosis of respiratory failure following surgery has reimbursement and quality of care implications. If it occurs post-procedurally, respiratory failure is classified as a patient safety indicator (PSI) when it occurs following elective surgeries.
On the other hand, the diagnosis and coding of post-procedural respiratory failure often results in a significant payment increase to hospitals since it is an MCC. If improperly diagnosed without firm clinical grounds, it may become the basis for regulatory or financial penalties affecting the hospital and the physician.
A patient who requires a short period of ventilator support that is usual or expected for surgical recovery does not have acute respiratory failure and it would not be a clinically valid diagnosis. A further difficulty arises because the use of terms in the postoperative setting that seem clinically innocuous to physicians such as pulmonary insufficiency (acute or unspecified) result in the assignment of codes that may also be classified as MCCs. To avoid improper code assignment and claim submission, encourage your physicians not to use such terms in the postoperative setting unless the patient has acute respiratory failure.
Clinical Validation
Both respiratory failure and post-procedural respiratory failure are lucrative recovery auditor contractor targets. Facilities should have a policy that governs the coding of any condition (including respiratory failure) not supported by clinical criteria in the medical record. To validate the diagnosis, the patient must meet the diagnostic criteria for respiratory failure and if post-procedural, there must be acute pulmonary dysfunction following surgery requiring non-routine aggressive measures.
Summary
Understanding the authoritative diagnostic criteria for acute respiratory failure empowers coders and documentation specialists to confidently recognize, validate, query, and compliantly code these conditions. The two basic types of respiratory failure are hypoxemic and hypercapnic, sometimes occurring in combination. This specificity is clinically important and should be encouraged but is not required for correct coding and reimbursement since unspecified respiratory failure is still an MCC.
The P/F ratio is a powerful diagnostic, prognostic, and clinical management tool since a P/F ratio < 300 indicates acute hypoxemic respiratory failure. However, the acute hypoxemic criteria (pO2/SpO2 and P/F ratio) must be applied with caution to the diagnosis of acute-on-chronic respiratory failure since both are frequently abnormal in the usual chronic baseline state.
Carefully consider the implications of diagnosing, coding and billing acute respiratory failure or pulmonary insufficiency, and whether it is a clinically valid diagnosis.
(C) Copyright 2019-2023 Pinson & Tang LLC